Celiac plexus neurolysis is a safe and effective tool for palliative pain management, with a relatively low rate of complications. Celiac plexus neurolysis should be offered to patients with abdominal malignancy as a key component of the multidisciplinary approach for control of intractable abdominal pain. Appropriate use of cross-sectional imaging knowledge, CT technique, and various adjunctive maneuvers are invaluable to ensure good results
Abdominal pain is a common debilitating problem in patients with abdominal malignancy and often dramatically affects quality of life and survival. Management of cancer-related abdominal pain is a complex and challenging issue and often necessitates chronic use of high-dose narcotic analgesics, which, in turn, are generally associated with several adverse effects.
The pain that originates from the upper abdominal viscera is carried by special visceral afferent fibers that relay through the splanchnic nerves and celiac plexus. The term celiac plexus refers to a network of nerve fibers located in the retroperitoneum, along the anterolateral wall of the aorta. An effective means of alleviating the intractable pain associated with abdominal malignancy is to disrupt nociceptive impulses at the level of the celiac plexus or splanchnic nerves. Imaging-guided celiac plexus block and neurolysis are invaluable therapeutic options for managing refractory abdominal pain and have been widely used since their introduction by Kappis et al in 1914.
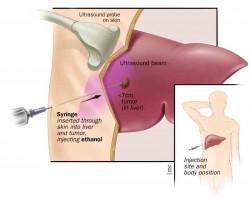
Although the terms celiac plexus block and neurolysis are used interchangeably, they differ in terms of duration of action. Celiac plexus block refers to temporary disruption of pain transmission via the celiac plexus and is accomplished by injecting corticosteroids or long-acting local anesthetics. In contrast, celiac plexus neurolysis, or neurolytic celiac plexus block, refers to permanent destruction of the celiac plexus with ethanol or phenol. Imaging guidance for celiac plexus neurolysis is most often performed with multidetector computed tomography (CT), which has superseded the use of fluoroscopy- or ultrasonography (US)–guided techniques. Despite its benefits and low complication rate, CT-guided celiac plexus neurolysis is generally underutilized.
Neurolytic celiac plexus block offers improved pain control, reduces the amount of narcotic analgesics, and has a lower incidence of constipation than standard treatment. The major benefit of celiac plexus neurolysis is in the reduced rate of analgesic consumption and lower incidence of drug-related adverse effects.
Indications
Imaging-guided percutaneous celiac plexus neurolysis is often performed in patients with persistent and intractable abdominal pain caused by pancreatic, gastric, esophageal, or biliary malignancy, as well as metastatic liver cancer and malignancy associated with retroperitoneal lymph node metastasis. It has also been reported to be beneficial in managing severe nausea and vomiting in patients with pancreatic cancer. This beneficial effect has been attributed to the effect of celiac plexus neurolysis on gastric motility, which increases peristalsis resulting from unopposed parasympathetic activity that arises from sympathetic denervation of the gastrointestinal tract. Celiac plexus block also provides relief from severe long-lasting abdominal pain in patients with chronic pancreatitis.
Contraindications
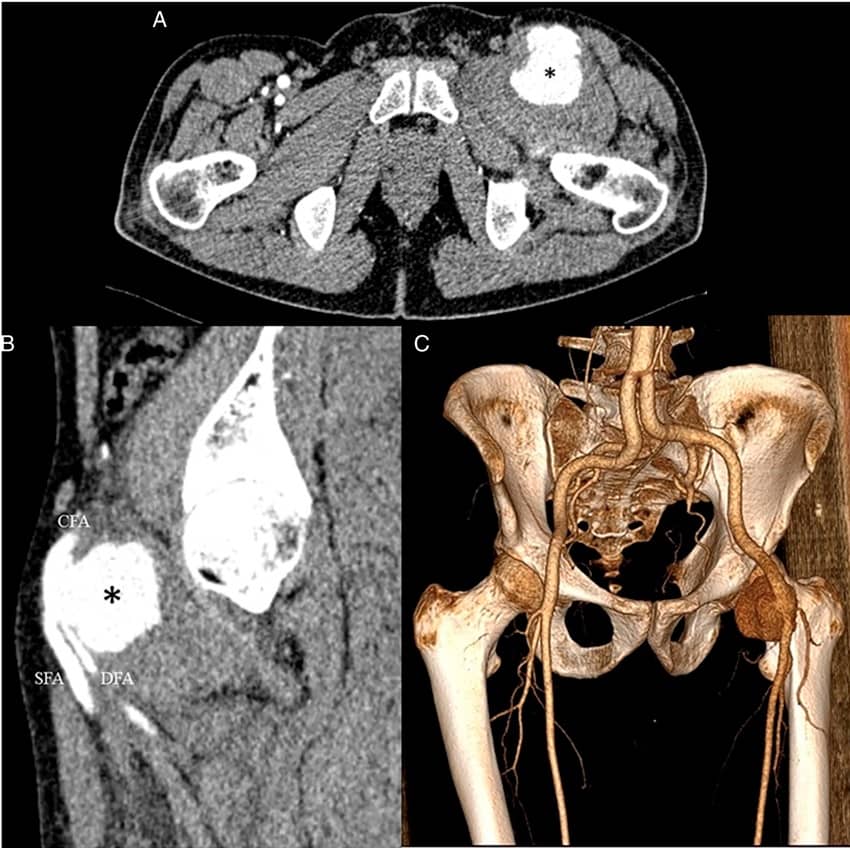
Although they are relative, several contraindications to celiac plexus neurolysis have been described. For instance, celiac plexus neurolysis is contraindicated in patients with severe uncorrectable coagulopathy or thrombocytopenia because of an increased risk for bleeding. Because of the close proximity of the celiac plexus to vascular structures, celiac plexus neurolysis is contraindicated in patients with abdominal aortic aneurysm, aortic mural thrombosis, or an eccentric origin of the celiac artery. A local or intraabdominal infection and sepsis are also contraindications for celiac plexus neurolysis. Because of its effect on bowel motility, celiac plexus block should be avoided in patients with bowel obstruction. An inability to visualize anatomic structures because of large soft-tissue masses obscuring the retroperitoneal fat planes is a relative contraindication for celiac plexus neurolysis.
Patient Preparation
Celiac plexus neurolysis is frequently performed in hospitalized patients with advanced cancer who are undergoing palliative treatment. When performing celiac plexus neurolysis on an outpatient basis, we generally prefer to admit the patient overnight for observation, particularly those who are debilitated and who have poor nutritional status because hypotension is common after the procedure. Before the procedure, patients should fast for at least 8 hours, and anticoagulants should be temporarily discontinued to minimize the risk for bleeding. Other medications should be continued in the preoperative period. Celiac plexus neurolysis is performed under intravenous conscious sedation with agents such as midazolam and fentanyl. Cardiorespiratory monitoring, including electrocardiography, blood pressure, and pulse oximetry, is an essential component of the procedure. Oxygen administration may be necessary in older or obese patients, particularly if the procedure is performed with the patient in the prone position.
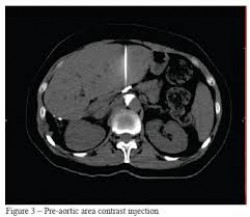
The first essential step in CT-guided celiac plexus neurolysis is preprocedure planning. Preoperative images must be reviewed in detail to determine the patient position, CT approach, needle entry site, needle path, and site of neurolytic agent injection. Meticulous planning ensures that the neurolytic agent is properly distributed in the antecrural space, enhances the analgesic effect of the procedure, and reduces morbidity.
Patient Position
Several different positions may be used depending on the CT approach and the patient's general condition. The most common positions are prone, lateral decubitus, supine, and oblique.
Bilateral Posterior Paravertebral Antecrural Approach
The bilateral posterior paravertebral antecrural approach is the most frequently performed approach for neurolysis. With this approach, the neurolytic agent is injected into the antecrural space by placing needles on each side by way of a posterior paravertebral route. Patients may be either in the prone or lateral decubitus position.
Anterior Approach
In the anterior approach, the patient lies supine, and the needle is inserted through the anterior abdominal wall and into the retropancreatic space. Because of the anatomic considerations with this approach, the needle often traverses the stomach, liver, or pancreas before reaching the celiac plexus.
Bilateral Posterior Paravertebral Retrocrural Approach
The bilateral posterior paravertebral retrocrural approach is mainly used to destroy the splanchnic nerves in the retrocrural space. Retrocrural splanchnic neurolysis is a reasonable alternative to the antecrural approach when the preaortic space is affected by anatomic distortions resulting from extensive tumor spread.
Posterior Transintervertebral Disk Approach
In this approach, the needle directly traverses the T12-L1 or L1-L2 intervertebral disk to reach a paraaortic location at the level of the celiac trunk. Reports describe a feeling of breakthrough when the needle breaches the anterior longitudinal ligament. The posterior transintervertebral disk approach may be performed unilaterally or bilaterally, and approximately 25–30 mL of neurolytic agent is injected once the needle tip is positioned in the antecrural space.
Diagram shows the trans-intervertebral disk approach for celiac plexus neurolysis, in which the needle traverses the intervertebral disk space lateral to the spinal cord.
Posterior Transaortic Approach
In the posterior transaortic approach, a single needle is passed through the posterior and anterior walls of the aorta by way of a left posterior paravertebral approach, a seemingly dramatic method that is relatively safe despite direct puncture of the aorta. However, before performing this procedure, accurate localization of the abdominal aorta and its visceral branches is imperative to prevent bleeding complications.
Direct Tumor Infiltration
This technique has been advocated for use in patients whose retropancreatic space is completely occupied by a primary tumor or metastatic lymphadenopathy and in whom optimal localization of the celiac plexus is difficult. In this method, multiple needles puncture the tumor mass at several points, followed by injection of a neurolytic agent into the mass, often with greater resistance than with injection into the retroperitoneal spaces.
Postprocedure Care
After the procedure is complete, we generally prefer to admit patients overnight for observation and to assess for immediate complications, particularly in patients who are elderly or with poor physical condition or nutritional status. In the immediate postprocedure period, patients are carefully monitored because of the high risk for hypotension. For this reason, patients should undergo bed rest for at least 12 hours after the procedure . Regular monitoring of cardiorespiratory status, including blood pressure, heart rate, and other vital signs, is crucial. Adequate fluid replacement in the form of intravenous fluids is performed as needed. In the immediate postprocedure period and on the day after the procedure, a focused neurologic examination is performed to determine if any neurologic complications are present. The success of celiac plexus neurolysis may be ascertained by assessing the patient's pain intensity (by using a scale of one to ten) and comparing the result with that obtained before the procedure. In addition to a subjective evaluation, objective assessment of pain improvement may be achieved by evaluating reductions in analgesic dosage after the procedure.
Complications
Percutaneous CT-guided celiac plexus neurolysis is a relatively safe procedure, with major complications reported in less than 2% of patients. Most of the reported complications are transient and minor when performed with CT guidance and with adequate local anesthetic or intravenous sedation provided before administration of neurolytic solution. Back pain is the most common complication, occurring in nearly 96% of patients, and is thought to result from neurolysis of sensory nerve fibers within the celiac plexus. Back pain usually radiates to the shoulder and may persist for up to 72 hr after the procedure. Shoulder pain likely results from diaphragmatic irritation. Anterior abdominal pain is uncommon after a posterior approach, and its presence should alert the interventionist to possible peritoneal irritation. Orthostatic hypotension is another common complication, affecting nearly 10%–52% of patients. Hypotension results from the decreased sympathetic tone, causing vasodilatation and relatively low blood volume and cardiac output. To minimize the risk for hypotension, patients are advised to undergo 12 hours of bed rest after the procedure. In addition, adequate fluid replacement with intravenous fluid is necessary to maintain an adequate blood pressure.
Transient diarrhea is a common complication of celiac plexus neurolysis, occurring in as many as 44% of patients. The mechanism for diarrhea resulting from celiac plexus neurolysis is not completely understood; however, it may be caused by decreased intestinal transit time and increased peristaltic activity resulting from unopposed parasympathetic activity, a result of blocked intestinal sympathetic efferent fibers. Diarrhea resulting from celiac plexus neurolysis is usually self-limiting in nature. Chronic diarrhea is rare and often refractory to treatment; its cause seems to be continued nerve injury by neurolytic agents. A few studies have reported that atropine and octreotide, a somatostatin analog, may be useful in managing chronic diarrhea resulting from celiac plexus neurolysis.
Other severe complications of celiac plexus neurolysis include neurologic injuries such as monoplegia and anal and bladder sphincter dysfunction, pneumothorax, arterial injury (eg, dissection), local hematoma, pleuritis, transient hematuria, pericarditis, intervertebral disk injury, and retroperitoneal abscess. Lower extremity paralysis with loss of bladder and bowel function is rare and occurs in less than 0.15% of patients. Neurologic complications usually result from inadvertent injection of neurolytic agent into the spinal artery that supplies the spinal cord, resulting in spinal ischemia. Another proposed cause of neurologic complications is subarachnoid injection of the neurolytic agent. Neurologic complications are uncommon when celiac plexus neurolysis is performed with CT guidance.


Leave a Reply
Want to join the discussion?Feel free to contribute!